Chiropractic & Back Pain
Chiropractic and Back Pain
 Low back pain is a very common pain symptom. One out of three of us suffer from some kind of back pain every year, and many people live with chronic spinal pain.
Low back pain is a very common pain symptom. One out of three of us suffer from some kind of back pain every year, and many people live with chronic spinal pain.
The good news is that chiropractic has been shown over and over to be an effective treatment of back pain. Here's a collection of articles that discuss how chiropractic can help in the treatment of back pain.
Watch our videos in the playlist below, or read some of our articles to learn more about how chiropractic can help ease back pain.
Back Pain After Auto Accidents
Back Pain and Chiropractic
Back Pain Treatments
Articles:
Aortic Calcification, Disc Degeneration, and Back Pain
Back Pain Assessment and Advice in Primary Care
Back Pain, Fibromyalgia, and the Stress Response System
Back Pain: General Information and Symptoms
Back Pain Recovery Can Be Slow
Childhood obesity linked to back problems
Don't Wait For Low Back Pain to Send You to the ER
Fear of Movement and Low Back Pain
Fear of Pain More Disabling than Actual Pain
Job Satisfaction and the Transition from Acute to Chronic Back Pain
Neck and Back Pain in Schoolchildren: The Role of Backpacks
Physical Risk Factors and Back Pain
Predictors of LBP and Return to Work
Prognostic Factors for Low Back Pain patients returning to work
Socioeconomic Impact of Back Pain
Stressful Life Events and Low Back Pain
Study shines light on who develops chronic low back pain
Waddell's Nonorganic Signs in Occupational Low Back Pain Patients
Whiplash or Fibromyalgia?
Whiplash or Fibromyalgia?
A recent study published in the journal Pain sheds some light on the ongoing debate about the causal relationship between neck injuries sustained during a car accident and the development of the pain condition fibromyalgia. Chiropractors commonly treat patients with both conditions, and separating these diagnoses can improve treatment. The latest research suggests that fibromyalgia may be overdiagnosed in patients who have a history of whiplash injury due to a motor vehicle accident.
People with fibromyalgia experience a range of life-disrupting symptoms, include general and localized pain, fatigue, and difficulty sleeping. Neck and shoulder tenderness is one common indicator that practitioners use to diagnose fibromyalgia; general pain lasting longer than three months is another. However, these symptoms also are common among patients experiencing the lingering effects of whiplash. Some past research has shown that people with neck injuries incurred in a motor vehicle accident are 13 times more likely to develop fibromyalgia than those with other injuries. Other studies have questioned these conclusions.
Researchers at the University of Washington set out to investigate the prevalence of fibromyalgia in whiplash patients with persistent neck pain. They questioned whether the most common set of criteria used for diagnosing fibromyalgia may rely too heavily on evaluating trigger points located in the neck and shoulder. The study participants included 326 individuals with whiplash-associated neck pain that had lasted longer than 3 months. The participants were enrolled in a 6-week treatment program for their symptoms that consisted of educational therapy sessions.
The researchers evaluated the patients for fibromyalgia both at the beginning and the end of the program. Two sets of criteria were used to diagnose fibromyalgia: the standard guidelines and adjusted guidelines that discounted the importance of pain in the neck and shoulder area. Using the standard guidelines, the researchers initially diagnosed 14% of the whiplash participants with fibromyalgia. This rate dropped to 8% using the adjusted guidelines.
These findings suggest that health practitioners who treat patients with persistent neck pain, such as chiropractors, may be led to significantly overdiagnose fibromyalgia in their patients. People with a history of whiplash-associated injuries should be aware of this unintended bias, and report their injury history.
Robinson JP, Theodore BR, Wilson HD, Waldo PG, Turk DC. Determination of fibromyalgia syndrome after whiplash injuries: Methodologic issues. Pain. 2011 Mar 16.
Motor Vehicle Accidents and TMD
Motor Vehicle Accidents and TMD
Few published studies have investigated the effect of temporomandibular joint disorders (TMD) and motor vehicle accidents. Since a correlation between the etiology of TMDs and trauma from vehicle accidents is controversial and undetermined, the researchers evaluated 50 files of patients with post-vehicle accident TMD. Evaluating the signs and symptoms, diagnoses, and outcomes, they found evidence explaining the possible effects of the two.
76% of the group identified TMD-related symptoms within one week or less of accident. Symptoms included TMJ or limited jaw opening, headache, neck and back pain. Since almost the entire sample experienced a rear-end or front-end collision, the researchers compared these two predominant groups.
The front-end collision patients reported jaw locking more frequently, and direct injuries to facial and dental areas; but the group required a fewer number of treatment types and experienced less tenderness over time.
Patients in the rear-end collision group were the opposite: they received more treatment types and reported masticatory tenderness during the final examination. Similarly, although the patients involved in severe vehicle accidents experienced more head, facial, and dental injuries, patients involved in minimal damage accidents reported more treatment visits and had higher rates of tenderness than with severe damage.
After assessing the accident and impact factors, the researchers found a slower recovery in those collisions with: minimal vehicle damage, lack of headrest use, poor driver position, and settlement of claim. This last finding is particularly interesting, as litigation is usually believe to prolong symptoms: "...insurance claim settlement at the time of the initial visit did not seem to suggest a better prognosis for patients with post-MVA TMDs..."
While discussing the onset of symptoms, the researchers concluded:
"We find it troubling that TMJ symptoms were identified by the patients themselves (rather than by health care providers) for over 80% of the study patients. Nondental health care workers must heighten their awareness of the possibility of TMD-related problems occurring in the MVA patient..."
Kolbinson DA, Epstein JB, Senthilselvan A, Burgess JA. Effect of impact and injury characteristics on post-motor vehicle accident temporomandibular disorders. Oral surgery, Oral Medicine, Oral Pathology 1998; 85(6):665-673.
Chiropractic Treatment of Spinal Fracture
Chiropractic Treatment of Spinal Fracture
Two recent studies have been published that discuss the successful management of spinal fractures with chiropractic treatment.
The first1 describes the case of a 49-year-old man who, after a fall on his buttocks, developed an "oblique (zone III) fracture through the fifth sacral segment with slight anterior displacement of the distal fragment."
"Neurological examination was unremarkable. On orthopaedic examination, the buttock pain was elicited by stressing the sacroiliac (SI) joints, but the distal sacral pain was not aggravated. Patrick's test was negative."
"Palpation revealed marked tenderness of the distal sacrum. Both SI joints were tender and hypermobile. Palpation of the lumbosacral and gluteal musculature did not recreate the patient's symptoms."
"After obtaining the patient's informed consent, the SI joints were manipulated with the patient in side-posture, once on each side, with a contact over the proximal SI joint. Interferential current was applied over the sacrum for analgesia. The patient felt markedly improved immediately."
Further chiropractic treatment consisted of four daily treatments, and then five more treatments during the next two weeks. At that time the patient was discharged.
In the second case2, the authors describe the case of a 18-year-old man with a Chance fracture of L3. The man was sitting in the middle rear seat of a car that hit a tree. He was taken by ambulance to the emergency room, where the resident physician told him that radiographic findings were normal. He reported low back pain and paresthesia in the left leg. He was given pain medications and sent home.
The patient had the same symptoms 3 days later, but was again told that everything was normal. An orthopaedic surgeon then evaluated the radiographs and diagnosed a "nondisplaced fracture of L3 confined to the posterior fourth of the vertebral body."
The patient was brought to the chiropractic physician twelve days after the accident. "The chiropractic interpretation of the radiographic examination contradicted the opinion verbally provided by the orthopedist at the hospital. Plain films demonstrated a Chance fracture of L3, extending from both laminae through the pedicles and transverse processes and continuing into the posterior-inferior portion of the vertebral body of L3, passing through the inferior end-plate. It was clear that there was a posterior displacement of the posterior-inferior aspect of the upper part of the L3 vertebral body."
After careful examination of radiographs and CT images, chiropractic treatment was instituted.
"After the second adjustment to L3, the paresthesia to the left leg had resolved and the low back pain had reduced considerably. The patient was adjusted on three occasions at L3 over the course of a week...Approximately 1 month after beginning chiropractic care, the patient reported that the leg symptomatology, including the uncontrollable knee flexion, was very much improved."
At four months after the accident, the patient had no paresthesia in the left leg, and had occasional minor low back pain.
The authors of both studies warn that extreme caution should be observed when working with severe spinal trauma. We recommend that those interested in these studies obtain complete copies for themselves.
- Steiman I, Grod JP. Spinal manipulation in a case of sacral fracture: presentation in a chiropractic office. Journal of the Canadian Chiropractic Association 1996;40(3):145-149.
- Plaugher G, Alcantara J, Hart CR. Management of the patient with a Chance fracture of the lumbar spine and concomitant subluxation. Journal of Manipulative and Physiological Therapeutics 1996;19(8):539-551.
Whiplash Symptoms - Low Back Pain
Whiplash Symptoms - Low Back Pain
Over the last 10 years, hundreds of studies have been done on the problem of whiplash, and most of those studies have focused on the most common symptom of the diagnosis: neck pain. This concentration of research has resulted in a clear understanding of how a rear-end collision can result in injury.
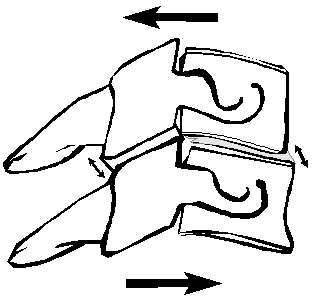
Shear forces occur when one part of the
spine moves in one direction while another
part of the spine moves in a different direction.
Shear forces can cause tearing or stretching
of the soft tissues that hold the spine together.
The primary reason why rear-end collisions cause injury is that the human spine is designed to withstand vertical forces, while a rear-end collision is a horizontal force. The vertical forces are known as “axial” forces. The horizontal forces, known as “shear” forces, cause unnatural movements of the cervical spine and can result in damage to the ligaments of the neck.
A new study has now shown that a similar injury mechanism occurs in the lumbar spine as well. Inspired by the research on the cervical spine, the authors of this study applied the same methodology to the low back.
They placed a cadaver in a standard automotive seat and placed acceleration-measuring devices in the vertebral bodies of T1, L1, L3, and L5. The seat was placed on a platform that was subjected to rear accelerations of 5g and 8g, or speeds of approximately 8 and 12 mph, respectively. The researchers collected acceleration data at a rate of 10,000 samples per second. Radiographs were taken of the spine before and after the tests.
The study found that different parts of the lumbar spine experience different strains during a rear-end impact:
“The anterior shear strains had mostly a biphasic response. Spinal strains started at about 30 msec after impact and peaked at the T12 vertebra at approximately 120 and 370 msec, whereas in the L4 vertebra, it peaked at 200 and 380 msec. The anterior strain patterns of the L4 and T12 vertebrae were in diametrically opposite directions.”
The direction and strength of the forces suggests that the car seat rapidly accelerates into the occupant’s spine, causing the thoracic and lumbar curves to straighten.
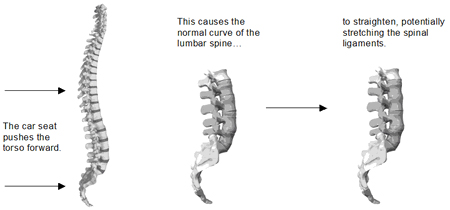
The authors of the study carefully examined the forces involved in the spine during the test impacts. They found that the car seat exerted about 1500 Newtons (approximately 337 pounds) of force, in a fraction of a second. The authors relate this to how the lumbar spine can be injured in rear end collisions:
“In the current study, no bony injuries were observed in the lumbar spine, either by visual inspection or by radiographic studies. In the absence of clear bony pathology after rear-impact collision, we propose that irritation of or injury sustained by the richly innervated spinal soft tissues (i.e., muscles, ligaments, capsules) plays an important role in the pathogenesis of lumbar pain after whiplash injury. This proposition is supported by work of others who performed lumbar spinal segment shear tests and showed that soft-tissue injuries occurred with a shear load as low as 1200 N.”
The 1500 Newtons of force was reached in the 5g test, which was equivalent to an 8 mph collision. So, according to this preliminary study, the car seat back exerts enough force during such a collision to injure the connective tissue of the lumbar spine.
Fast A, Sosner J, Begeman P, et al. Lumbar spinal strains associated with whiplash injury. American Journal of Physical Medicine and Rehabilitation 2002;81:645-650.
Whiplash, Referred Pain and the Central Nervous System
Whiplash, Referred Pain and the Central Nervous System
The most frequent symptoms after whiplash injury are headache and neck pain, which are understandable, since the neck is directly injured during a rear-end collision. Many auto injury patients, however, experience a much wider range of symptoms. Arm pain, shoulder pain, back pain, TMJ pain, and dizziness are also very common symptoms, and these are difficult to ascribe to direct trauma. A new study shows us that these other symptoms are actually related to the initial neck trauma, through the process of referred pain.
Referred pain is pain that is perceived in one area, but that originates in another. Researchers believe that referred pain occurs when pain signals from injured tissue activate adjacent nerves in the spinal cord or brain. These adjacent nerves then cause the brain to perceive pain in the area of the body innervated with those nerves.
Referred pain can be induced, even in pain-free people. In a new study from Sweden, researchers set out to determine whether whiplash patients had a different referred pain response to stimulus than non-whiplash subjects.
The authors started with 12 patients and 12 pain-free control subjects. Referred pain was created by electrical stimulation of the shoulder and the upper arm. The electrical stimulation level was set by the test subjects, and was adjusted to create five progressive levels of pain – innocuous, pain threshold, 2 out of 10, 4 out of 10, 6 out of 10 (on a scale of 1 to 10).
The results showed a dramatic difference between patients and controls:
- Pain-free subjects required almost three times more stimulation to reach the designated pain levels than did the whiplash subjects.
- While the controls reported limited areas of referred pain, the whiplash patients reported a much wider area of referred pain.
- Whiplash patients showed a unique type of referred pain. In healthy individuals, induced referred pain was always distal to the stimulation (or further from the center of the body), but in the whiplash patients, half of the patients had referred pain that was proximal to the stimulation.
These findings are important in understanding the nature of whiplash injuries. As previous studies have shown, some whiplash patients demonstrate “central hypersensitivity,” a phenomenon where the central nervous system becomes over-stimulated from the injury to the spine.
According to the literature, a certain percentage of patients are susceptible to chronic pain after an auto injury. In these patients, central nervous system changes may develop in reaction to pain, which can, in turn, increase the patient’s sensitivity to pain. It is critical to identify these patients early on after injury, in order to break this cycle. Sensory tests, such as pressure pain threshold testing, are an important diagnostic tool, since they can help us identify those patients with a posttraumatic stress reaction.
Kosek E, Januszewska A. Mechanisms of pain referral in patients with whiplash associated disorder. European Journal of Pain 2008;12:650-660.
Multidisciplinary Treatment For Chronic Whiplash
Multidisciplinary Treatment For Chronic Whiplash
The purpose of this study was to assess the effectiveness of a multimodal treatment program for patients with chronic symptoms after whiplash. 26 patients (13 male, 13 female) participated. All had experienced whiplash at least six months before the study and had experienced symptoms for an average of 20.8 months. All were partially or completely unable to work and had been absent from work for an average of 15.7 months.
A multidisciplinary team assessed all patients before treatment began. An orthopedic surgeon or neurologist conducted a full physical exam and assessed radiographs including extension-flexion films of the cervical spine. A physical therapist looked at cardiorespiratory fitness. Psychological assessment using MMPI-2 was done by a clinical psychologist. Neuropsychological screening was also done. An occupational therapist assessed the physical and mental demands of each patient's work. These assessments were used as baseline data to be compared with outcome data. Results of these assessments were shared with patients (and their partners) before the treatment program began.
Patients participated in a daily 4-week outpatient multimodal treatment aimed at restoring normal daily function. The patients were instructed to not use analgesics. It was explained that the purpose of the study was not to reduce pain, per se, but to increase regular functioning- including return to work. The program included physical training meant to end inappropriate pain behavior, restore muscle endurance and strength and to improve aerobic fitness. Group sessions were employed to discuss patient's deeply held beliefs on symptoms and disability.
Program outcome was measured using both self-report & objective criteria. Self-report measures included neck pain, headache, disability, fatigue, "vague" somatic symptoms, psychological distress, depression, and problems with concentration and memory. Objective measures looked at features of daily functioning such as return to work, drug usage, and medical consumption.
A six-month follow up assessment documented the program outcome. Statistically significant improvements on self-report measures were found. For somatic symptoms, 73% of patients fell within normal range. 96% rated within normal limits for psychological distress. 46% of patients were within normal health distribution for pain intensity (reportedly, nearly pain free). This improvement in pain levels occurred despite the fact that the treatment goal did not include pain reduction, and many of the activities required in the program could have increased pain. Follow up assessment of objective criteria showed a complete return to work for 65% of patients and at least partial return to work for 92% of patients. 81% of patients did not seek medical care during the follow up period. Only 58% of the patients reported no use of analgesics.
While improvement was noticeable in a segment of the test subjects, there were still a number of patients with pain symptoms. The authors address this issue:
"As has been established for chronic low back pain, cognitive behavioral treatment appears to be a promising treatment for patients with chronic symptoms after a whiplash injury. However, considering that more than 50% of patients did not show a clinically significant change and 35% of patients did not achieve a complete return to work, it is clear that there is still a great deal of work to be done. The question is, why did some patients not improve?"
The authors suggest that patient beliefs are responsible for chronic whiplash symptoms, and they refer to the severely flawed Quebec Task Force and the Lithuanian studies as evidence that there are no physical reasons for chronic pain. The study completely ignores the vast body of literature on whiplash biomechanics that isolate the cervical facet joints as a cause of pain after whiplash injuries.
Vendrig A, van Akkerveeken P, McWhorter K. Results of a multimodal treatment program for patients with chronic symptoms after a whiplash injury of the neck. Spine 2000;25(2):238-244.
Subcategories
Back Pain After Auto Accidents
Back Pain After Auto Accidents
Browse our articles to learn about conditions caused by automotive accidents.










